The numbers are staggering. Nationally, there was a nearly 30% increase in drug overdose deaths from February 2020 to February 2021. And in Colorado, the overdose death count rose by 40% during that time.1
It begs the question…If there was a 30% increase in the number of deaths from any other cause – diabetes, heart disease, cancer – would the status quo remain? Or would we be quick to promote and prescribe an FDA-approved drug shown to have significant positive impacts on outcomes?
Unfortunately, this scenario is the reality for opioid use disorders (OUD). The FDA has approved buprenorphine, methadone, and naltrexone for the treatment of OUD, yet, in 2019, only 18% of people with OUD in the United States received any of these lifesaving treatments.2 And roughly 40% of counties in the US did not have a single waivered provider able to prescribe these medications.
Clearly, we need to address the barriers that prevent access to this evidence-based care for opioid and other substance use disorders (SUD).
Why MAT?
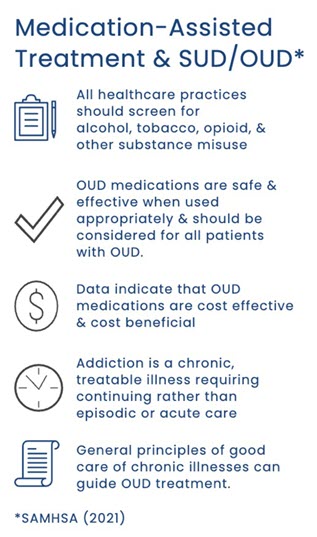
Medication-assisted treatment (MAT) is a life-saving, evidence-based treatment for SUD/OUD that will be vital to fighting the deadly opioid epidemic. But addressing SUD/OUD isn’t just about lowering the number of overdose deaths – treatment for SUD/OUD improves patients’ quality of life, reduces the rate of other chronic illnesses, and decreases morbidity and mortality from any cause. And in an increasingly value-based environment, it will be essential for clinics to identify and address both SUD and OUD in their patient populations.
How?
While methadone must be administered in a SAMHSA-certified treatment program, buprenorphine can be prescribed and dispensed within a much broader scope of settings, such as physician offices.
This has contributed to primary care becoming a critical factor in addressing barriers to care that exist and expanding access to treatment. But why primary care? It is, in part, because these providers and practices…
- Have established healing relationships and understand their patients’ care needs.
- Are experts in dealing with chronic and comorbid health conditions.
- Are less stigmatizing settings than addiction clinics.
But how could we put one more thing on primary care providers’ already overflowing plates? That is where team-based care comes into play. The whole of implementing a comprehensive MAT program does not fall on a lone clinician but, rather, can be supported by MAs, office staff, social workers, billing managers, and anyone else working within a clinic.
And at HealthTeamWorks, we have seen the impact of the OUD crisis, witnessing the effect it can have on the primary care practices and providers with whom we work. Because of this, we have implemented a number of efforts to help the medical community combat the crisis they are facing, working to:
- Increase the number of waivered providers able to prescribe buprenorphine for the treatment of OUD by deploying our MAT trained facilitators into practices throughout Colorado and beyond.
- Enhance the knowledge, skills, and comfort surrounding SUD/OUD and MAT to implement a team-based approach through training for all clinic staff – not just clinicians.
- Address the stigma within healthcare that creates barriers to SUD/OUD treatment by providing behavioral health allyship development.
Primary care is the heart of our nation’s healthcare system and a key to combatting the nation-wide opioid epidemic. And empowering these providers to address SUD/OUD will save saves, increase quality of life, and improve the health and wellbeing of individuals and communities. But asking practices to take on another responsibility without additional support may seem unrealistic at times. So, we are dedicated to providing and advocating for such support so that primary care teams can take on this critical challenge using evidence-based solutions.
If you or your organization would like to learn more about how HealthTeamWorks can support your efforts to address SUD/OUD, please reach out to solutions@healthteamworks.org
For additional details on MAT, SAMHSA released a comprehensive document on medications for OUD for providers, policymakers, patients, and families: Medication for Opioid Use Disorder
References
- Ahmad, F., Rossen, L., & Sutton, P. (2021). Provisional drug overdose death counts. National Center for Health Statistics. Available at https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- The PEW Charitable Trusts. (2021). Policies Should Promote Access to Buprenorphine for Opioid Use Disorder. Available at https://www.pewtrusts.org/en/research-and-analysis/issue-briefs/2021/05/policies-should-promote-access-to-buprenorphine-for-opioid-use-disorder









