Telemedicine: Is this your time to THRIVE with a new approach to delivering healthcare or are you just hoping to SURVIVE the disruptive innovation forced upon you and your patients with the move to virtual visits? It is acknowledged that virtual healthcare delivery was not a choice for most physicians, providers, staff and patients. We all suffer from the instinctive response to resist change, but as we also know ‘out of chaos comes new innovation and opportunities’ if we remain open to it and allow it. What will your perspective and desire be toward telemedicine in healthcare when the coronavirus crisis settles?
As I am doing my online weight class this morning, I am reminded how my view of virtual classes has evolved. Initially, I lamented missing in-person class... I really like my in-person instructor team and class. This is what I was comfortable with and doing this virtual thing, especially initially, was different and awkward. When we first went virtual, finding the correct site, making all the connections and ensuring audio was good created many challenges, but this feeling of chaos and discomfort has resolved. Now I have a link that works well, I can get to my class in under five minutes and am ready to go in much less time than it took to go to my gym. As I reflected on this, I realized I actually really like my virtual class, it has many positive attributes. The convenience allows me to workout more often (or for longer), the scenery (ocean and mountains) provides a positive impact on my mood toward the class, the variety of instructors brings value and the core of what I need, which is effective cues and motivation. The instructors love what they are doing and it is evident in the virtual version. I recognize that they too probably prefer in-person classes, but they have communicated only enthusiasm for this as an option. We share a common goal, to have a good workout.
There are similarities between everyday life that has now become virtual and the pros/cons of telemedicine.
As we move past the discomfort of figuring out all the technology pieces, are we as healthcare leaders stepping back and seeing the value add that telemedicine brings to our approach to healthcare delivery for our patients? Ensuring quality of care for our patients is why we do what we do. If we do not take time to objectively see this, we miss an opportunity to thrive in this time of disruptive innovation and we are at risk of conveying our discomfort with the experience, when our patients are looking to us for reassurance.
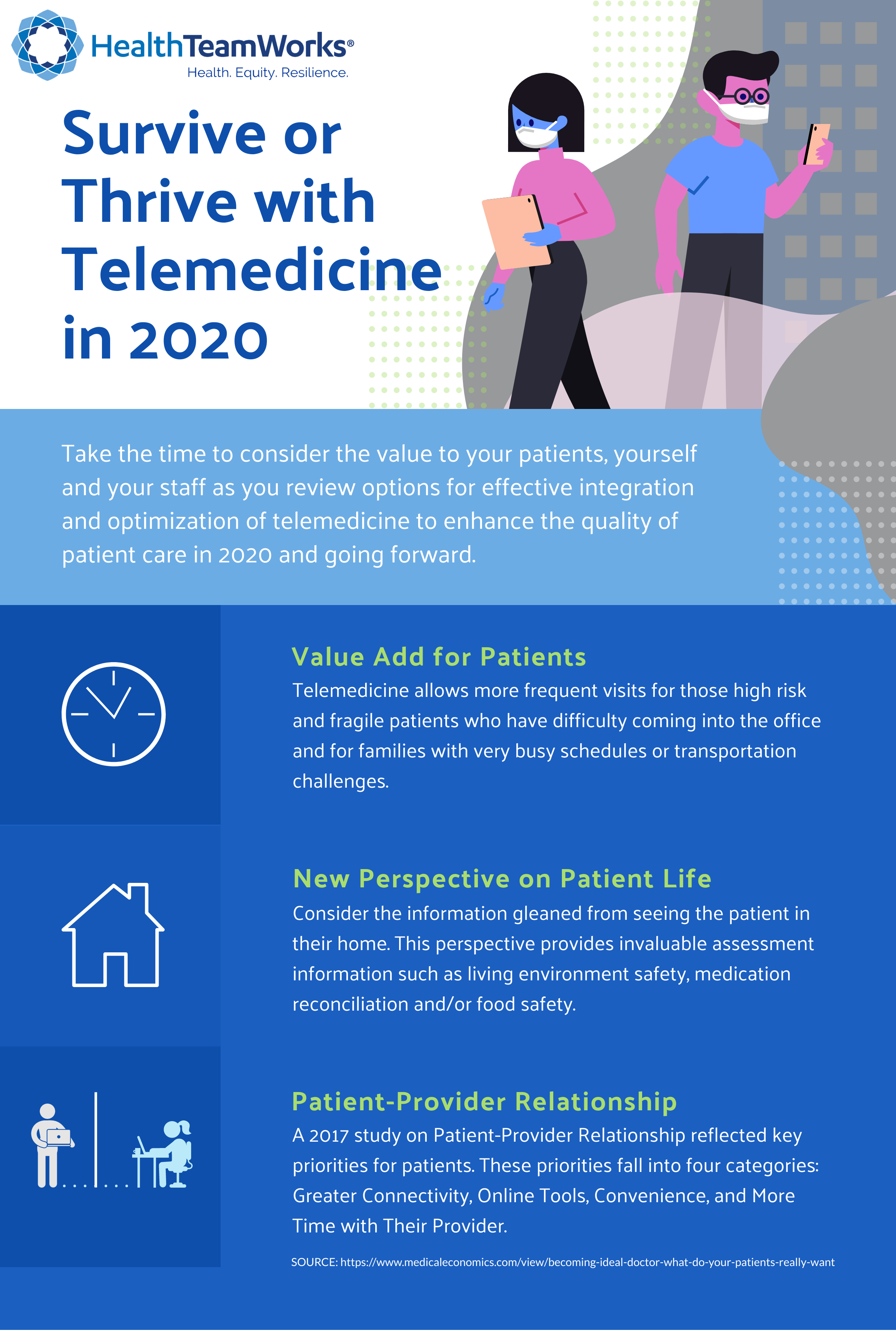
Have we taken the time to truly appreciate the value add for our patients with telemedicine?
-
Consider the convenience for the patient (and for providers) that allows more frequent visits, especially for high-risk and fragile patients who have difficulty coming into the office, and for families with busy schedules or transportation challenges. Have we considered the time it takes for our patients to come into our office for a visit? Many primary care providers have seen younger patients use online visits over the past several years. They want and demand convenience and are willing to forego continuity. Consider experiencing the convenience of a virtual visit for yourself or family member and see what the patient view is like. The convenience of not having a 15-30 minute (minimum) travel time to the clinic is amazing for those with a busy schedule. Not to mention that the patient can be doing things in their home instead of waiting restlessly in a waiting room if the provider is not exactly on schedule (I know that never happens in primary care). The convenience of being able to participate in a visit with an elderly family member who lives eight hours away can be invaluable for all involved.
-
Consider the information gleaned from seeing the patient (elderly as well as young) in their home. This perspective provides invaluable assessment information such as living environment safety, medication reconciliation (when you can see the plastic bins or shoe boxes of pill bottles that they have), and/or food safety when you can see a view of their kitchen or eating area. This can more than make up for the lack of face to face time for some visits. The value of seeing a patient in their home setting brings back the days of home visits that some have yearned for. The awareness of home setting compliments the patient-provider relationship in many ways.
Have we as healthcare leaders (physicians, providers and staff) looked closely at our attitude towards telemedicine? This ‘attitude’ can significantly impact how our patients perceive the use of telemedicine now and going forward.
Do we work to communicate the positives and the value of the virtual visit or do we repeatedly bring up or complain about the challenges of technology or the desire to seeing them in-person (without acknowledging the value of seeing them in their home)?
Does our communication style reflect enthusiasm and embracing this new opportunity (thriving) or do we communicate a surviving attitude? The impact of body language and communication style is unchanged whether virtual or in-person, and it speaks loudly.
Do we as healthcare providers and staff communicate the ability to build and maintain an effective relationship with the patient so that they feel more comfortable with the virtual option? The core of what patients want is trust in their healthcare team and quality of care. As with many components of an effective patient-provider relationship, provider/staff attitude can make it or break it!
A 2017 study on Patient-Provider Relationship (participants age 21-70) in three regions of the country showed that what patient want most fall into 4 categories:
-
Greater connectivity – they want to be able to reach their provider when they need medical information or attention. Call it greater connectivity or access, patients want to talk with you when they need it. Virtual or telephonic options enhance this and meet their needs.
-
Online tools – patients are getting more accustomed to online resources. How many of us have used an application on our phone for FaceTime, Skype, now Zoom, banking or other convenience-based interactions. A 2015 Health Consumer Adoption survey showed that 8 out of 10 internet-connected adults have used at least one digital health tool. Let’s partner to ensure these are quality tools that meet our patients’ needs virtually.
-
Convenience – even before the coronavirus pandemic of 2020, patients wanted convenience. The option of virtual visits is key to meeting this need moving forward.
-
More time – patients would much rather have that time they use to drive to a clinic to interact with their provider, consider this benefit to the patient visit.
Numerous studies have sited components such as provider compassion, convenience, high quality care and time with my provider as key attributes of what patients want from their primary care provider. Not one study that I reviewed stated a physical exam or in-person visit as a priority for the patient. Consider this as you move forward.
I hear a lot about the elderly not liking technology and I respond by asking ‘how many of us feel that physical activity is good for our elderly patients?’ Isn’t mental activity equally (if not more) important to our elderly patients? I taught my 90-year-old father-in-law to use an iPhone just prior to the coronavirus pandemic and it was a life saver for both him and his loved ones. I will never again even think that the elderly do not want to learn something new. My father-in-law and his family continue to FaceTime on a daily basis. He, with the help of his local library, was able to download audio books and he loves to see the pictures of his grandchildren, great grandchildren and soon to arrive great great grandchildren. The social isolation of the coronavirus pandemic would have been devastating without technology. We walk together virtually, listen to books together and share music preferences, something we could not do without technology due to the physical distance between us. We were able to bridge the physical distance and ensure a strong connection. He insisted his primary care provider and cardiologist do virtual visits via technology for his safety and peace of mind. This was not without some challenges at first, like frequent pocket dials to all of his family, calling wrong numbers because he could not see the numbers, and his frequent calls to us to figure out how to do things, but the challenges are so worth the benefits we see now. Our reassurance that he is doing ok as we can see him at home (or at the walking track), he has social interactions most days of the week (while maybe not in-person, like we all prefer, virtual provides safety for him), he has been challenged mentally (which is as beneficial as his new walking program), and he is proud of his accomplishments (he is the star of his social distance coffee group as he has the newest iPhone and he is teaching others how to use their phones).
Consider these basic needs prior to judging your patients’ (of all ages) ability to master technology.
-
Do your patients need effective resources? ….Yes
-
Do they need coaching and time to figure it out? ….Yes
-
Do we as physicians, providers and staff set the environment for thriving or surviving the disruptive innovation of telemedicine use in healthcare delivery? A resounding yes.
There are certainly other factors that are likely top of mind (e.g. internet access, payment for telemedicine, etc.). Hopefully you will take the time to step back and consider the value to your patients, yourself and your staff as you envision a culture of effective integration and optimization of telemedicine that enhances the quality of care to your patients in 2020 and going forward.
Written by Diane Cardwell, MPA, NP, PA-C, Practice Facilitator at HealthTeamWorks
Resources:
-
Jim Higgins, "Becoming the ideal doctor: What do your patients really want?" Medical Economics. February 7, 2018, https://www.medicaleconomics.com/view/becoming-ideal-doctor-what-do-your-patients-really-want
-
"The Patient-Provider Relationship Study: The Ripple Effect Starts with Boomers", Solutionreach, 2017, https://www.solutionreach.com/rethinking-the-patient-provider-relationship
-
"Digital Health Consumer Adoption: 2015", Rock Health, 2015, https://rockhealth.com/reports/digital-health-consumer-adoption-2015/









