August 29, 2005 Hurricane Katrina made landfall leaving severe damage from New Orleans, LA to Biloxi, MS. The Category 3 storm brought 127 mile per hour winds, heavy rains, and surging Gulf waters. In its wake an estimated 1,577 people perished in Louisiana - fifty-one percent Black and forty-nine percent over 75 years old (Brunkard, PhD, Namulanda, MS and Ratard, MD, 2008) - due in great part to the catastrophic failure of the levees in Lake Pontchartrain. Largely, these lives lost represented a group of immobile poor who stayed in place either because they were physically or financially unable to evacuate, or because they lacked trust in the entities tasked with protecting public safety. All these factors are indicative of structural inequities across the United States leading to disparate impact and compromised health outcomes.
Fifteen years out from Katrina, the poverty, questionable allocation of public resources, rates of chronic illness, and stark racial segregation survived the storm. I ended a call last week with a community partner in New Orleans by checking in on how she is navigating the healthcare space as our country deals with a new crisis - COVID-19. She said somberly, “…more people have died here from COVID-19 than from Hurricane Katrina.” A stark and apt juxtaposition, given that fifty-eight percent of the 1,697 who have died from COVID-19 related causes in Louisiana are Black people according to the Louisiana Department of Health (Department of Health, State of Louisiana, 2020).
City after city… New Orleans, New York, Chicago, Detroit, even my hometown of Kansas City, MO, have reported disparity in rates of COVID-19 illness among Black people and Latinos. As the data rolls in, more community groups are asking that reporting be made available based on gender, age, racial, ethnic, and socio-economic indicators.
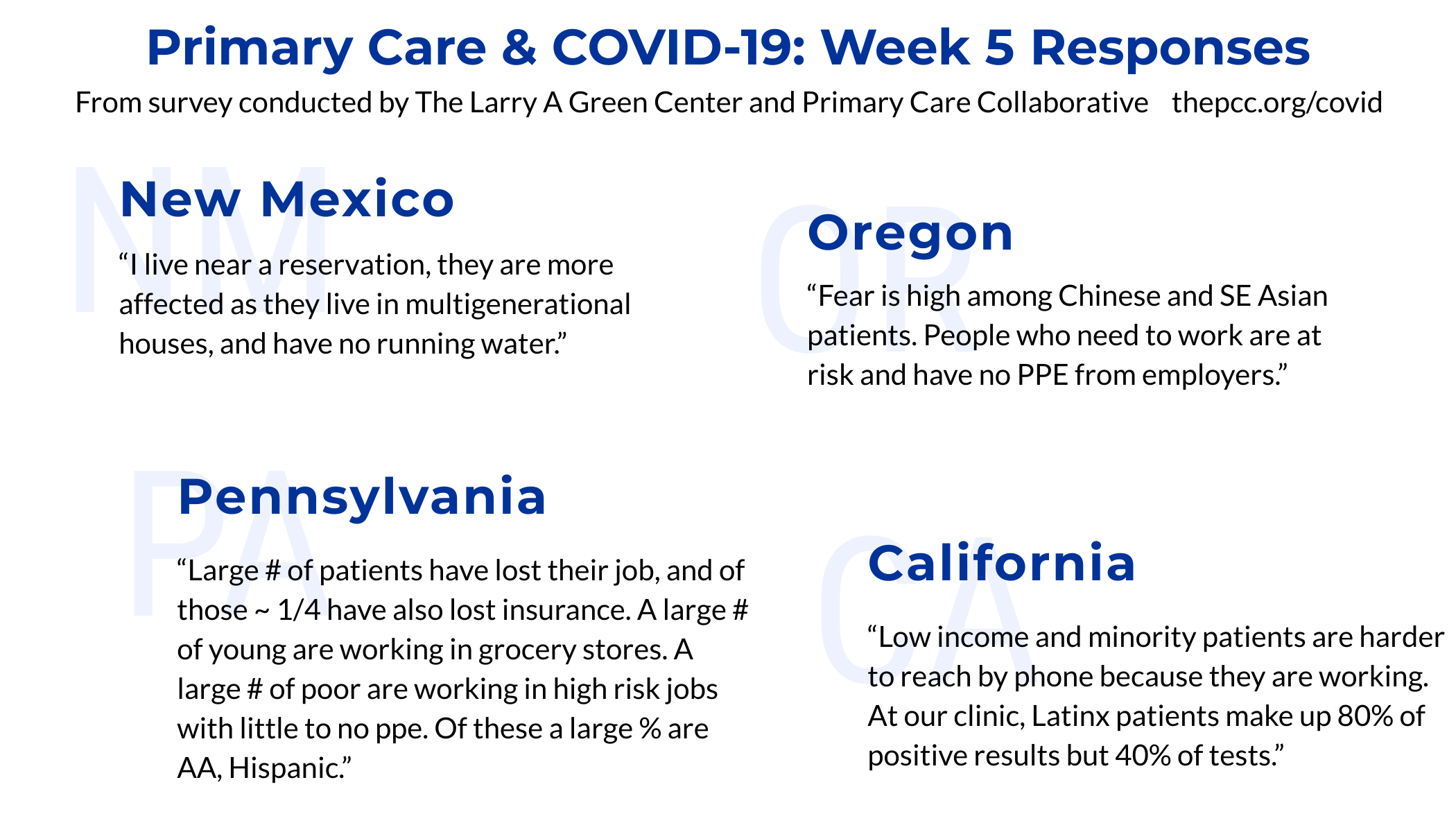
On April 17, The Larry A. Green Center and Primary Care Collaborative’s “Quick COVID-19 Primary Care Survey: Series 5 Executive Summary” relayed that 70 percent of responding clinicians reported trends in COVID-19-related health disparities and burdens (Larry A. Green Center and Primary Care Collaborative, 2020).
As of April 26, The Centers for Disease Control and Prevention’s (CDC) nationwide data shows thirty percent of COVID-19 patients are Black and thirty-one percent are Latino, despite making up around thirteen and nearly seventeen percent of the national population respectively (Coronavirus Disease 2019 (COVID-19) in the U.S., 2020). The COVID storm is also leaving catastrophic mortality rates in its wake for those Black and Latino patients struggling to recover from the illness. Yet, the data is incomplete, and a full picture is only beginning to emerge.
Why? That is the question on the minds of the people and communities impacted, public health agencies, and providers of care. It is convenient to blame the patient for these higher rates of infection and poorer outcomes. Things like higher rates of co-morbidity, for example, are quickly rattled off to explain the imbalance as if they sufficiently sum up the matter at hand. This approach oversimplifies the issue to a discussion on how much the doctor can do to help the “non-compliant patient”. We cannot accept the easy answer for this complex quandary that translates into lives lost needlessly with each natural and epidemiological disaster. The why, and how to address it, will only be defined when communities impacted, public health agencies, and healthcare organizations build coalitions to strive for the best solutions and commit to the uncomfortable conversations required. Having witnessed what existing partnerships like these have started to unearth, we found frequently referenced drivers for health equity that we will draw inspiration from in a series of blogs and peer forum discussions:
- Acknowledging, Measuring and Addressing Disparate Impact (CO Office of Health Equity, 2020)
- Mobilized People and Communities
- Culturally Congruent Policies (Payne, 2020)
- Early Childhood Development
- Housing Sanitary and Safety Requirements
- Just Employment and Working Conditions
- Equitable Universal Access
We invite you to engage in these conversations with us over the coming weeks as we take on different perspectives regarding the impact of health inequity on our well-being as a nation. We hope to expand understanding of structural inequity and use what we know to make sure future resources take into account these issues.
Sign in or join HealthTeamWorks' Solutions Center for free. Then visit our Peer Forum “Structural Inequity” to contribute to the discussion.
Written by Cecilia L. Saffold, COO, HealthTeamWorks
References:
Brunkard, PhD, J., Namulanda, MS, G. and Ratard, MD, R., 2008. Hurricane Katrina Deaths, Louisiana, 2005. [online] Ldh.la.gov. Available at: <https://ldh.la.gov/assets/docs/katrina/deceasedreports/KatrinaDeaths_082008.pdf> [Accessed 27 April 2020].
Centers for Disease Control and Prevention. 2020. Coronavirus Disease 2019 (COVID-19) In The U.S.. [online] Available at: <https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html> [Accessed 27 April 2020].
Department of Public Health and Environment. 2020. Office Of Health Equity. [online] Available at: <https://www.colorado.gov/pacific/cdphe/ohe> [Accessed 29 April 2020].
Larry A. Green Center and Primary Care Collaborative, 2020. Quick COVID-19 Primary Care Survey Series 5 Fielded April 10 - 13, 2020. [online] Primary Care Collaborative. Available at: <https://www.pcpcc.org/sites/default/files/news_files/C19%20Series%205%20National%20Executive%20Summary.pdf> [Accessed 27 April 2020].
Ldh.la.gov. 2020. Louisiana Coronavirus COVID-19 | Department Of Health | State Of Louisiana. [online] Available at: <https://ldh.la.gov/coronavirus/> [Accessed 27 April 2020].
Payne, Hakima Tafunzi., 2020. Culturally Congruent Care In A Community Setting. [online] Available at: <https://www.facebook.com/HakimaTafunzi> [Accessed 27 April 2020].









