Bonnie T. Jortberg, PhD, RD, CDE; Douglas H. Fernald, MA; L. Miriam Dickinson, PhD; Letoynia Coombs, EdD; Nicole Deaner, MSW; Caitlin O’Neill, MS, RD; Frank deGruy, MD; Larry Green, MD; W. Perry Dickinson, MD
BACKGROUND AND OBJECTIVES: The patient-centered medical home (PCMH) is a practice model that is intended to improve the quality of care by making it safer, more comprehensive, integrated, and personal. However, most family medicine residency programs are not fully prepared to train residents on this idealized model. The Colorado Family Medicine Residency PCMH Project’s overall objective is to transform 10 residency practices into PCMHs through practice improvement and curriculum redesign. This paper focuses on the programs’ implementation of key PCMH components into the residency curricula and the impact on resident self-perceived competence in and use of PCMH components.
METHODS: Mixed-method evaluation assessed PCMH curricular characteristics, routine use of PCMH components in patient care, and perceived resident competence after implementation of quality improvement coaching and PCMH curriculum tools. Baseline and follow-up PCMH semi-structured curriculum interviews assessed elements included in the residency programs’ curricula. The PCMH Clinician Assessment (PCMH-CA) Survey assessed routine use of PCMH components in patient care. The PCMH Competency Self-Assessment Survey assessed residents’ perceived competency in applying PCMH elements in patient care.
RESULTS: Qualitative data results demonstrated active efforts by the residency programs to implement key PCMH components. Survey results showed significant improvement from baseline to follow-up (12–36 months).
CONCLUSIONS: Implementation of the key components of PCMH into practice improvement efforts and residency curricula improved residents’ routine use of PCMH in patient care and their perceived PCMH competence.
(Fam Med 2014;46(1):11-18.)
The patient-centered medical home (PCMH) is a practice model that is intended to improve the safety, comprehensiveness, coordination, and personal nature of health care rendered to primary care patients. The major primary care organizations developed joint principles to describe and endorse the characteristics of the PCMH,1 and the model has received a great deal of attention as a way of increasing quality and decreasing costs of health care.2-5 However, most primary care practices are poorly prepared to deliver this idealized model and need extensive changes to fully accomplish improvements in care. Lessons learned from major practice change efforts are that this sort of practice change is very difficult, takes longer than anticipated, and requires assistance and additional resources to accomplish.6,7 It is critical that primary care residency programs serve as exemplars in this area, since clinical training during residency strongly influences future practice patterns, and residents will need leadership and practice improvement skills to foster and support practice transformation in their future practices.8
Current residency education does not incorporate many of the PCMH elements. In 2004, an Institute of Medicine report on implementing successful medical innovations noted, “Clinical education has not kept pace with, or been responsive enough to, shifting patient demographics and desires, changing health system expectations, evolving practice requirements and staffing arrangements, new information, a focus on improving quality, or new technologies.”9 The Future of Family Medicine report encouraged development of the PCMH model and specifically called for a period of intense innovation in family medicine residency education to enhance the capacity to produce physicians capable of effectively practicing in the PCMH and leading this transformation process.10 However, there are multiple variations in how practices and residency programs implement PCMH principles.11
The Colorado Family Medicine Residency PCMH Project had a goal to transform the nine Colorado family medicine residency programs and 10 residency practices into PCMHs through practice improvement and curriculum redesign.11 This project was a collaborative effort between the University of Colorado School of Medicine, Department of Family Medicine; HealthTeamWorks (a Colorado-based nonprofit practice support organization); the Colorado Association of Family Medicine Residencies; and the Colorado Institute of Family Medicine, with funding from the Colorado Health Foundation.
Key aims for the project included implementing key PCMH components into residency curricula and facilitating curriculum redesign efforts. The evaluation aimed to answer two questions: (1) What effect does the engagement of family medicine residency practice in PCMH changes have on residents’ perceived and self-reported competencies in PCMH and (2) What lessons can be learned that might guide other residency programs on this journey? This paper reports on implementation of PCMH curriculum changes and outcomes related to residents’ reported use of PCMH elements in patient care and perceived PCMH competency.
Methods
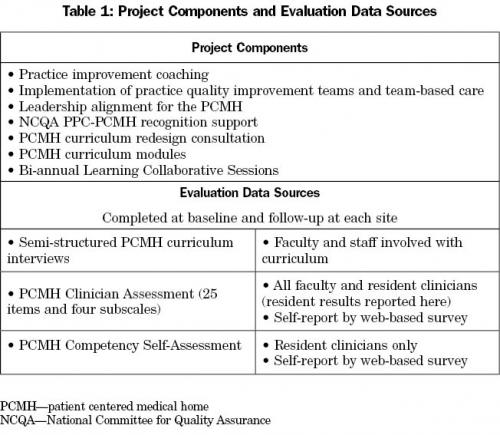
Our project used a prospective observational mixed-method evaluation to assess the intervention, with the project structure and data sources for the evaluation summarized in Table 1.
PCMH Intervention
Practice Support. Quality improvement (QI) coaches worked individually with practices to facilitate quality improvement efforts. Practice coaching has been shown to be effective in helping practices make the changes required for optimal program implementation,12 but has not been tested specifically for practice or curricular redesign in residency practices.13 QI coaches and other project staff also assisted with the NCQA PPC-PCMH recognition process, leadership alignment, and training within the practice. Practices participated in twice yearly learning collaborative meetings to share practice and curriculum redesign experiences. The project provided funding for practice coaching, assistance for curriculum redesign, participation in the bi-annual Learning Collaboratives, and other technical support to assist with PCMH transformation efforts.
Curriculum Support. Initial assessment of program coverage of PCMH topics was performed at baseline, including the PCMH Competency Self-Assessment by residents and the PCMH Curriculum Interviews described in detail below. A report of this assessment was provided to each program and used to plan curricular changes to better incorporate PCMH topics in the curriculum and provide residents with experiences in key areas. Curriculum redesign consultants worked collaboratively with each program to integrate the PCMH competencies into the curriculum and to create supervised resident experiences as leaders in the QI process; the project team also helped develop tools and specific PCMH curricula. Curricular topics were also covered in the learning collaboratives.
Protections. This evaluation project was reviewed by the Colorado Multiple Institutional Review Board and approved as exempt from human subjects research review.
Participants and Sites. All nine Colorado family medicine residencies and 10 practices participated. One residency has nine residents per class, three have eight residents per class, four have six residents per class, and one has six residents per year in the core program and four per year in a community health center track. All programs are in metropolitan areas (population 50,000 or more), with seven in primary care health professional shortage areas. The programs vary in patient populations, but most care for large percentages of Medicaid and uninsured populations. One program was a participant in the Preparing the Personalized Physician for Practice (P4) Project.14 At the beginning of the project just three of the 10 practices had a fully implemented EHR. During the 3-year project, four practices initially implemented EHRs, two practices changed to new EHRs, two upgraded to new versions, and the remaining two prepared for initial EHR implementation.
PCMH Measures
We used a mixed-method evaluation to assess baseline practice PCMH characteristics from multiple perspectives.
Interviews and Qualitative Data Analysis. Nine semi-structured PCMH Curriculum Interviews of faculty and staff were conducted with each program, assessing the program’s baseline and 3-year follow-up coverage of core PCMH components and competencies. Baseline interviews helped to determine “gaps” in the curriculum related to PCMH. The key PCMH components were Population Management, Information Systems, Team Approach, Coordination of Care, Quality Improvement, Patient Centeredness, Personal Physician, and Leadership Skills. Interviews included faculty and staff involved in each program’s curricular design. The same investigator performed baseline and follow-up interviews for each residency. Interview results provided contextual data about implementation of PCMH components in the programs and practices.
The interviews were audio recorded and transcribed. An iterative process was used to identify and refine themes around PCMH curriculum redesign, with the interviewer initially rating the training needs for each PCMH curricular area immediately after interviews. Our qualitative analysis team met regularly to review data as it was collected. Team members individually immersed themselves in the data to identify themes and then met to discuss each other’s analyses to identify common themes. Investigators went through cycles of reading, summarizing, and re-reading the data. The senior author then over-read and verified the results based on the transcriptions.
Survey Data and Statistical Analysis. Surveys were administered at initial engagement with practice coaching activities and again at the end of the 3-year project, with the period between survey administrations ranging from 18 to 30 months.
(1) The PCMH Clinician Assessment (PCMH-CA) survey of residents assessed their routine use of the PCMH components as part of patient care. The PCMH-CA was derived from two previously developed instruments, the Assessment of Clinician Depression Management and the Assessment of Clinician Diabetes Management, which assess clinician use of elements of the chronic care model.8 Previous versions have been shown to be related to improvements in diabetes outcomes in two studies, one not yet published.15 Items were adapted to be appropriate across chronic diseases, and items were added to assess other PCMH concepts. PCMH-CA results were analyzed using principal factor analysis with oblique rotation, retaining factors as determined by the proportion criterion. Cronbach’s alpha was computed for each subscale to confirm internal consistency. Subscale scores were computed and used as outcome variables in the analysis of change over time. The final PCMH-CA version included 25 items and four subscales. Subscales were scaled to a 0 to100 range, with higher scores corresponding to higher degrees of implementation of or competency in the PCMH model.
(2) The PCMH Competency Self-Assessment measured residents’ perceived competency in applying the PCMH elements in patient care, using a set of PCMH resident competencies developed during the initial stages of this project and since used by other residencies and projects for designing PCMH curricular redesign.
Initially, means, standard deviations, and frequency distributions were examined for all measures and surveys. The structure of the data was hierarchical, with respondents nested within practices. Because surveys were anonymous, pre and post data could not be linked to individuals, only practices. Multilevel models (general linear mixed models) with random effects for practice were used to examine pre-post differences in PCMH-CA scales (Team-Based Clinical Systems Redesign, Information Systems, Patient Centeredness, and Self-Management Support). Only one independent variable was included in each model, an indicator variable for pre- versus post-time effect. Demographic information was not collected and thus no covariates were included. Intraclass correlations for residents within practices were as high as 0.131, confirming the need for multilevel models with adjustment for clustering. In the first analysis, the outcome variable consisted of scores on the PCMH-CA scales. In the second analysis, the outcome variable consisted of scores on scales from the Resident PCMH Competency Self-Assessment Survey. Statistical analysis was performed using SAS version 9.3 (SAS Institute, Cary, NC).
Results
Interview Data
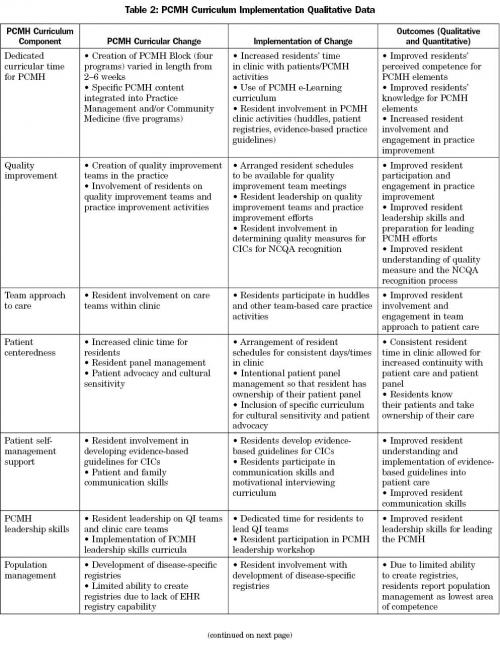
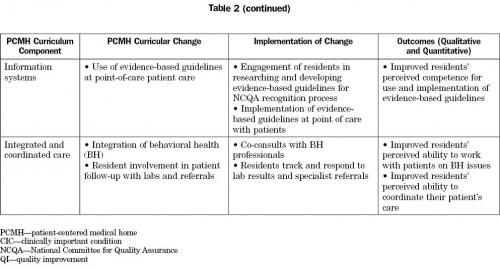
Interviews with residency faculty and staff revealed themes regarding program implementation of PCMH elements. Programs identified several areas for further development, including the need for dedicated curricular time for the PCMH, flexibility in scheduling to include residents in QI efforts in the clinic, involvement of residents in developing a team approach to care, training in techniques for patient self-management support, development of resident leadership skills, and resident involvement with the development and use of patient registries and population management. Faculty also identified a need for faculty development, as many of the PCMH components were not something that faculty were trained in or currently teaching or practicing. Faculty also expressed a concern that they did not have the time or resources to develop specific PCMH curricular content.
The baseline assessment guided programs in key changes that positively influenced implementation of PCMH curricular components and identified curricular needs at the onset of the project. This led to the development by our team and the programs of specific curricula, materials, and trainings related to these areas.
Dedicated Instructional Time. Although programs were teaching some aspects of PCMH in the curriculum at baseline, they were not labeled as such, and programs realized that intentional teaching time needed to be dedicated to PCMH teaching (didactic sessions, clinic experiences, precepting, etc). There were similarities and differences in how programs accomplished dedicated time. Four of the programs set aside blocks of time for specific PCMH teaching, varying from 2 weeks each year of residency training to a 4-week block during the second year of residency training. Five programs chose to integrate PCMH components into their existing community medicine or practice management curricula. There were common elements in both approaches, including increased resident clinic time, resident projects related to PCMH, resident involvement on the QI teams, use of the PCMH e-Learning curriculum modules described below, and didactic sessions that related to PCMH.
Project Support for PCMH Curriculum Development. To assist programs with specific curricular content and materials for PCMH, our team developed an e-Learning PCMH curriculum, a web-based tool that utilized the PCMH competencies developed by our team. The e-Learning curriculum comprised 12 specific PCMH modules and offered programs flexibility regarding how they could choose to integrate the modules into their curricula. Interestingly, the PCMH e-Learning curriculum also became a faculty development tool, utilized by several programs as a way for their faculty to learn more about PCMH.
Leadership Development. Our assessment identified the development of resident skills in leadership for practice redesign as a crucial need. In addition to leadership in the PCMH e-Learning curriculum, our team developed a PCMH leadership skills workshop. Residents (and sometimes faculty) from each program participated in this workshop. Specific PCMH leadership skills addressed included developing a shared leadership model (less hierarchical than traditional leadership), staff engagement, development of team-based care, and leading teams through change.
QI Team Participation. Another important PCMH curricular component implemented by all programs was the involvement of residents on QI teams developed through the practice improvement part of the project. Eight of the 10 programs instituted QI teams that met twice per month. One program that did not implement practice-wide QI teams involved residents in disease-specific QI efforts. Programs expressed difficulty with residents’ consistent participation on QI teams due to competing time demands, which became an issue for curricular redesign. Some programs involved residents in their NCQA PPC-PCMH recognition application: specifically, they researched guidelines for clinically important conditions and developed patient self-management tools. Although all programs struggled with population management due to difficulties extracting patient registry data from their EHRs, all programs involved residents with EHR implementation including clinical decision support and work flows. Residents were involved in team-based care activities, including huddles and the formation and implementation of team-based care within the practice. There was agreement on the areas of relative strength and weakness both within interviewees for each program and across programs. Specific PCMH curriculum implementation approaches and outcomes are described in Table 2.
Survey Data
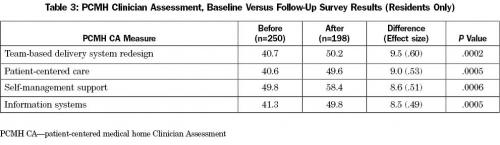
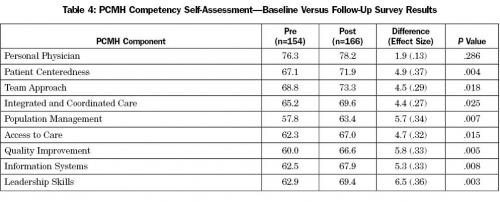
Patient-Centered Medical Home Clinician Assessment (PCMH-CA). Results of analyses of PCMH-CA subscales over time are included in Table 3.
Residents reported statistically significant increases in routine use of all PCMH components as part of patient care (P<.01). It is important to note that the relative level of use of PCMH components was low across the categories, with none of the areas near the 100-point ideal (average post-score = 53.77).
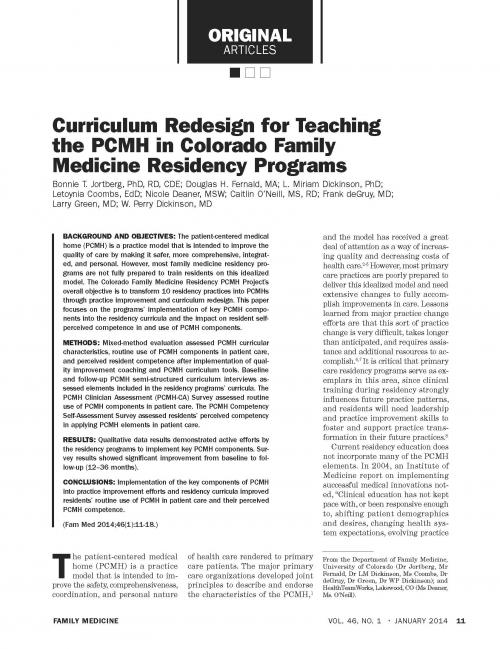
PCMH Competency Self-Assessment. Results from the pre and post resident scores for the PCMH Competency Self-Assessment also showed statistically significant increases in scores for all domains (P<.05) except for Personal Physician; however, this domain had the highest pre-survey score (76.3 compared with 63.4 as mean pre-score for the other domains). Results for the PCMH Competency Self-Assessment are shown in Table 4.
Discussion
The results from three different PCMH assessment approaches indicated that key PCMH components can be implemented into family medicine residency curricula. This improved residents’ routine utilization of PCMH components in patient care and residents’ perceived PCMH competency. These improvements required that residency programs modify the residency curricula. Modifications across all programs included resident involvement with practice QI teams, PCMH leadership development, project support for PCMH curriculum development, and intentional and dedicated PCMH teaching time. Programs were able to accomplish this through different methods of either creating blocks of PCMH teaching time or integrating key PCMH concepts into already existing curricula. Freeing up residents for consistent time to participate with QI teams and take active participation and leadership proved to be difficult for all of the programs.
Although integration of PCMH principles into residency education is an emerging area of study, other researchers have also been able to show significant changes in resident attitudes after implementation of PCMH concepts. Evan et al found that residents’ attitudes toward chronic pain patients significantly improved after participation in a PCMH innovation curriculum.16 A retrospective study demonstrated that alumni ratings of the practice-based curriculum increased following implementation of the PCMH model, which included resident use of a clinical quality management system to proactively manage patients with chronic conditions and to address prevention/health maintenance issues.17
Several key issues and lessons learned regarding development and implementation of a PCMH curriculum into family medicine residency education were identified in our project. Intentional and dedicated time is needed to successfully implement the key PCMH components into residency curricula. Experiential learning through active participation on the QI teams and other practice QI efforts are also keys to their learning. Given current family medicine residency requirements, this can be challenging but not impossible to accomplish. Specific training for PCMH leadership skills is also necessary, since this requires a different model of leadership.
Another key to the success of PCMH curriculum implementation was project support for development of PCMH curricular materials and teaching tools. Development of specific PCMH curricular educational materials is time-consuming and something for which faculty may have neither the time nor expertise to accomplish. Consequently, development of the PCMH e-Learning curriculum proved instrumental in enabling programs to implement key PCMH components. Lastly, faculty development for the PCMH is crucial, as many have not been taught these concepts nor do they currently practice them as part of patient care.
This project was funded as a redesign project for all Colorado family medicine residency programs, not as a research project, so that a randomized design was not possible, limiting our ability to ascribe program changes only to the intervention. However, at the time of this project, many PCMH concepts were not part of routine family medicine curricula, and most programs were not working actively on PCMH implementation. A potential limitation of these results is that self-reported levels of competency in or implementation of PCMH components may be artificially inflated in some areas due to a lack of understanding of the intricacies of the PCMH model. This could be particularly evident in concepts such as team-based care and patient centeredness, since most clinicians initially think that they already work well in teams and are patient centered. Corroboration of the key patterns of strengths and weaknesses through interviews helped in overcoming this limitation. An additional limitation is that this evaluation only assessed residencies in one state, and Colorado programs could be different in some ways than those in other states. This is also an evaluation of limited domains and for a short time interval. The long-term goal is to determine if these curricular changes result in different practices, different approaches to QI, and better patient care.
Conclusions
Results of our evaluation indicate that implementation of key components of PCMH into practice improvement efforts and residency curricula improved residents’ routine use of PCMH in patient care and their perceived PCMH competence. Further investigation is needed to fully understand best practices as this field continues to evolve.
ACKNOWLEDGMENTS: The Colorado Health Foundation provided funding for this work.
CORRESPONDING AUTHOR: Address correspondence to Dr Jortberg, University of Colorado, Department of Family Medicine, Mail Stop F496, AO1, 12631 E. 17th Avenue, Room 3519, Aurora, CO 80045-0508. 303-724-0973. Fax: 303-724-0977. bonnie.jortberg@ucdenver.edu.
References
- American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP), American Osteopathic Association (AOA). Joint principles of the patient-centered medical home. 2007. https://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. Accessed November 9, 2010.
- Grundy P, Hagan KR, Hansen JC, Grumbach K. The multi-stakeholder movement for primary care renewal and reform. Health Aff (Millwood) 2010;29(5):791-8.
- Margolius D, Bodenheimer T. Transforming primary care: from past practice to the practice of the future. Health Aff (Millwood) 2010;29(5):779-84.
- Reid RJ, Coleman K, Johnson EA, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29(5):835-43.
- Steiner BD, Denham AC, Ashkin E, Newton WP, Wroth T, Dobson LA Jr. Community care of North Carolina: improving care through community health networks. Ann Fam Med 2008;6(4):361-7.
- Crabtree BF, Nutting PA, Miller WL, et al. Primary care practice transformation is hard work: insights from a 15-year developmental program of research. Med Care 2011;49 (Suppl):S28-S35.
- Crabtree BF, Nutting PA, Miller WL, Stange KC, Stewart EE, Jaen CR. Summary of the National Demonstration Project and recommendations for the patient-centered medical home. Ann Fam Med 2010;8 Suppl 1:S80-S90, S92.
- Dickinson WP. Residents as change agents in the transformation of primary care practices. Fam Med 2010;42(7):469-70.
- Council NR. Academic health centers: leading change in the 21st century. In: Press TNA, ed. Washington, DC, 2004.
- Gorey TM, Kahn NB, Thomas S, McMillen MA. The future of family medicine: a collaborative project of the family medicine community. Ann Fam Med 2004;2:S3-S32.
- Fernald DH, Deaner N, O’Neill C, Jortberg BT, deGruy FV III, Dickinson WP. Overcoming early barriers to PCMH practice improvement in family medicine residencies. Fam Med 2011;43(7):503-9.
- Baskerville NB, Liddy C, Hogg W. Systematic review and meta-analysis of practice facilitation within primary care settings. Ann Fam Med 2012;10(1):63-74.
- Nutting PA, Crabtree BF, Stewart EE, et al. Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Ann Fam Med 2010;8 Suppl 1:S33-44, S92.
- Carney PA, Eiff MP, Saultz JW, et al. Aspects of the patient-centered medical home currently in place: initial findings from preparing the personal physician for practice. Fam Med 2009;41(9):632-9.
- Nutting PA, Dickinson WP, Dickinson LM, et al. Use of chronic care model elements is associated with higher-quality care for diabetes. Ann Family Med 2007;5(1):14-20.
- Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med 2010;363(6):501-4.
- Pugno PA, McGaha AL, Schmittling GT, DeVilbiss Bieck AD, Crosley PW, Ostergaard DJ. Results of the 2010 National Resident Matching Program: family medicine. Fam Med 2010;42(8):552-61.
From the Department of Family Medicine, University of Colorado (Dr Jortberg, Mr Fernald, Dr LM Dickinson, Ms Coombs, Dr deGruy, Dr Green, Dr WP Dickinson); and HealthTeamWorks, Lakewood, CO (Ms Deaner, Ms. O’Neill).
| Attachment | Size |
|---|---|
| 254.08 KB |