Care coordination involves intentionally organizing patient care activities, sharing information with all health care professionals involved in the patient's care, ensuring safe transitions across care settings, and timely post-acute follow-up. The cost of fragmented care is high, not only from a financial standpoint, but also in increased risk to the patient.
At its core, effective care coordination can improve outcomes for everyone: patients, providers, and payers. This section will focus on coordinating care within the primary care practice and across providers, services and settings, including coordination within the medical neighborhood and community. It will also cover strategies for a community needs assessment based on a defined population and demographics.
Collaborative agreements are verbal or written compacts between a Primary Care Provider and a referral source that specify the types of patients referred, types of referral, consultation, or co-management arrangements available. They further define testing to be completed prior to referral, availability for “curbside consults", and who is accountable for which processes and outcomes of care.
Guide
Co-Management is the act of collaborating in the delivery of care for shared patients between the Primary Care Provider and Specialty Care Provider(s) when the necessary care and treatment is beyond the scope of the Primary Care Provider. This process is useful to:
Guide
Overview
Protocols for care coordination are guidelines designed to streamline processes commonly used during care coordination activities. Protocols define a common set of procedures for all providers, staff, patients and referral sources that result in:
Guide
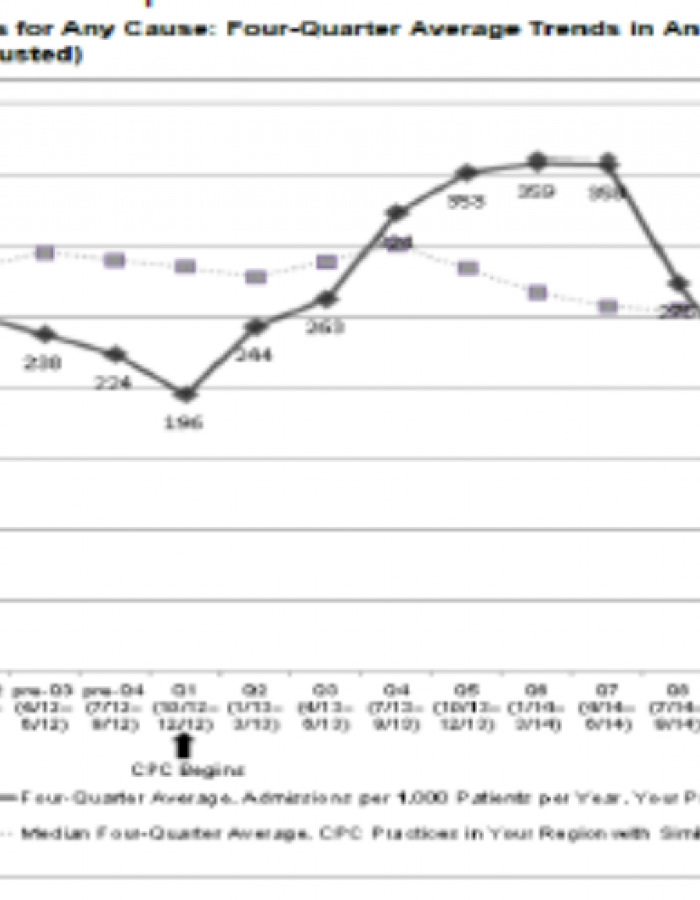
Practice Credits 63% Drop in ACSC Admissions to ‘Going All In’
UC Health – Timberline Medical, Estes Park, Colorado; system-affiliated; 3.5 providers; 3,900 patients